Abstract

Introduction: Acquired thrombotic thrombocytopenic purpura (aTTP) is a rare, life-threatening thrombotic microangiopathy, in which accumulation of ultra large von Willebrand factor (ULvWF) multimers leads to an increased risk of thrombus formation in small blood vessels due to platelet adhesion. A combination of plasma exchange (PE) and immunosuppression is the current mainstay of treatment for aTTP. The efficacy of caplacizumab in aTTP patients, in conjunction with PE and immunosuppression, was demonstrated in both placebo-controlled Phase II TITAN study and Phase III HERCULES study. Herein, we present the results of the integrated efficacy analyses of both studies.
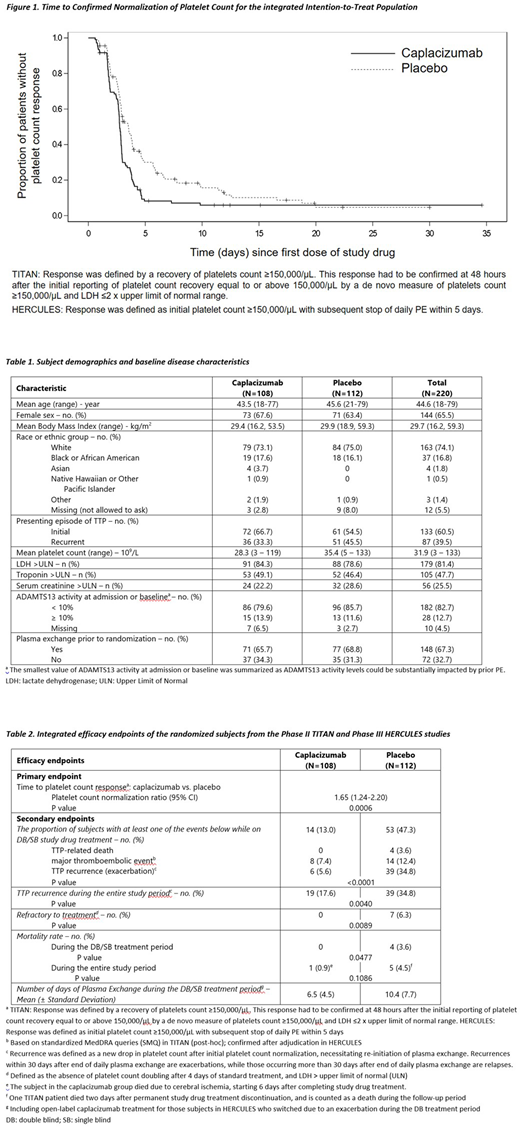
Methods: All randomized patients in the TITAN and HERCULES studies were integrated and included in the analysis population. Patients had a single-blind (SB, TITAN) or a double-blind (DB, HERCULES) treatment period followed by a follow-up period of 30 days. Patients in the HERCULES study could enter an open-label treatment period (i.e., in case of exacerbation during the DB treatment period). The primary endpoint was time to platelet count response, analyzed according to the corresponding platelet count response definition for each individual study (Figure 1). Secondary endpoints included: (i) the proportion of patients with TTP-related death, a recurrence of TTP, or at least one treatment-emergent major thromboembolic event; (ii) the proportion of patients with a recurrence of TTP during the DB/SB treatment period and the overall study period; (iii) the proportion of patients with refractory TTP (defined as the absence of platelet count doubling after 4 days of standard treatment, and LDH above normal); (iv) mortality rate during the DB/SB treatment period and the overall study period; (v) the number of PE days during the DB/SB treatment period.
Results: 220 patients were randomized in both studies, 108 to the caplacizumab group and 112 to the placebo group. The groups were balanced with respect to demographics and baseline disease characteristics except for an imbalance relating to a history of previous TTP episode (Table 1). There was a statistically significant difference in favor of caplacizumab in time to platelet count response (p <0.001; platelet count normalization rate ratio [95% CI] of 1.65 [1.24, 2.20]) (Figure 1, Table 2). Treatment with caplacizumab resulted in a 72.6% reduction in the percentage of patients with TTP-related death, a recurrence of TTP, or at least one treatment-emergent major thromboembolic event during the DB/SB treatment period compared to placebo (p <0.0001) (Table 2). Treatment with caplacizumab resulted in an 84.0% reduction in the percentage of patients who had a recurrence of TTP during the DB/SB treatment period (p <0.0001), and a 49.4% reduction in recurrences during the overall study period (p <0.005), compared to placebo (Table2). No patients in the caplacizumab group had refractory TTP during the DB/SB treatment period compared to 7 patients (6.3%) in the placebo group (p <0.01) (Table 2). There was a statistically significant lower rate of death in the caplacizumab group (no deaths) compared to the placebo group (4 deaths) during the DB/SB treatment period (p <0.05) (Table 2). During the overall study period, one patient randomized to caplacizumab died (during the treatment-free follow-up period, judged unrelated to caplacizumab by the Investigator), compared to 5 patients randomized to placebo (Table 2). During the overall treatment period, there was a reduction in the mean number of PE days of 3.9 days in the caplacizumab group compared to the placebo group (Table 2).
Conclusions: This integrated efficacy analyses confirmed results from the individual Phase II and III studies showing that treatment with caplacizumab significantly reduces the time to platelet count response compared to treatment with placebo. In addition, treatment with caplacizumab was associated with clinically meaningful and statistically significant reductions in: (i) the proportion of patients with TTP-related death, a recurrence of TTP, or at least one treatment-emergent major thromboembolic event; (ii) the proportion of patients who died from TTP during the study drug treatment period; (iii) the proportion of patients with a recurrence of TTP during treatment and overall; (iv) the number of patients refractory to therapy; (v) the mean number of days of plasma exchange.
Peyvandi:Kedrion: Consultancy; Roche: Speakers Bureau; Octapharma US: Honoraria; Kedrion: Consultancy; Ablynx: Other: Member of Advisory Board, Speakers Bureau; Roche: Speakers Bureau; Sobi: Speakers Bureau; Sobi: Speakers Bureau; Octapharma US: Honoraria; Sobi: Speakers Bureau; Roche: Speakers Bureau; Grifols: Speakers Bureau; Roche: Speakers Bureau; Grifols: Speakers Bureau; Novo Nordisk: Speakers Bureau; Shire: Speakers Bureau; Ablynx: Other: Member of Advisory Board, Speakers Bureau; Grifols: Speakers Bureau; Grifols: Speakers Bureau; Roche: Speakers Bureau; Kedrion: Consultancy; Ablynx: Other: Member of Advisory Board, Speakers Bureau; Kedrion: Consultancy; Ablynx: Other: Member of Advisory Board, Speakers Bureau; Novo Nordisk: Speakers Bureau; Sobi: Speakers Bureau; Shire: Speakers Bureau; Novo Nordisk: Speakers Bureau; Octapharma US: Honoraria; Novo Nordisk: Speakers Bureau; Novo Nordisk: Speakers Bureau; Ablynx: Other: Member of Advisory Board, Speakers Bureau; Shire: Speakers Bureau; Shire: Speakers Bureau; Shire: Speakers Bureau; Octapharma US: Honoraria; Grifols: Speakers Bureau; Sobi: Speakers Bureau; Octapharma US: Honoraria; Kedrion: Consultancy. Cataland:Alexion: Research Funding; Shire: Consultancy; Ablynx: Consultancy, Other: Member of Advisory Board. Scully:Novartis: Honoraria, Other: Member of Advisory Board, Speakers Bureau. Coppo:Ablynx: Consultancy. Knöbl:Ablynx: Consultancy, Other: Member of Advisory Board. Kremer Hovinga:Shire: Other: Member of Advisory Board, Research Funding; Ablynx: Other: Member of Advisory Board. Metjian:Ablynx: Other: Member of Advisory Board. De La Rubia:Ablynx: Consultancy, Other: Member of Advisory Board. Minkue:Ablynx: Employment. Callewaert:Ablynx: Employment. De Winter:Ablynx: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal